Manténgase sano!
- Nora R. Miller, MD, infertility specialist at Yale Medicine's Greenwich Fertility
- Posted May 18, 2023
Infertility in Men and Women: Its Causes and Treatments
Infertility can be a heartbreaking experience for couples who are desperate to have children, but doctors can help them figure out why they can't conceive and then treat the problem.
Infertility is defined as the inability to conceive after 12 months of unprotected intercourse. If the woman is 35 or older, then she is considered infertile after six months of trying without getting pregnant.
Primary infertility is when the woman has never been pregnant. Secondary infertility is when the woman has conceived in the past, but now is having difficulty doing so. One in six couples face infertility.
The first step is to acknowledge there is a problem and seek professional guidance.
Usually, a reproductive endocrinologist will perform an evaluation if infertility is suspected. This includes testing both partners.
Tests for male infertility
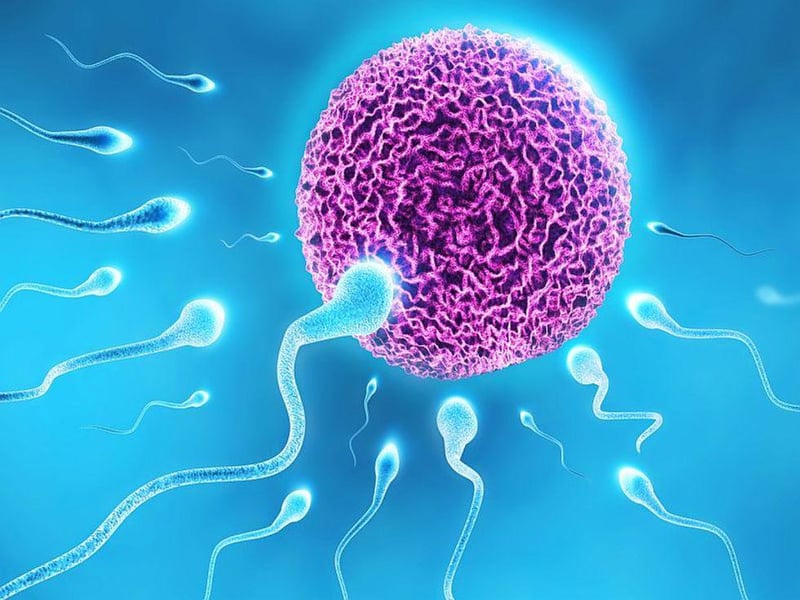
The male partner should undergo a complete semen analysis. This analyzes the semen volume, count, motility and morphology.
A normal volume confirms that the man's ejaculatory system is connected. The presence of sperm confirms that he is fertile. The motility determines what percentage of his sperm are alive after one hour. Lastly, morphology involves the shapes of the sperm. Only a small percentage of sperm are normally shaped and able to fertilize eggs.
Tests for female infertility
The female partner undergoes a hormonal evaluation, including testing her thyroid and prolactin (the milk hormone that should only rise while pregnant or breastfeeding). Her ovarian reserve is assessed with anti-mullerian hormone which determines, in a crude manner, the quantity of her eggs. Follicle-stimulating hormone determines the quality of her eggs and is tested at the beginning of her menstrual cycle.
An ultrasound exam is also performed to assess the uterus and ovaries. Specifically, looking at the ovaries to determine the antral follicle count (the number of eggs available to grow during the current cycle) and to check for abnormalities (cysts, for example). The uterus is measured and checked for abnormalities (such as fibroids).
Next, a hysterosalpingogram is conducted. It's a noninvasive way of assessing the uterine cavity for abnormalities and the fallopian tubes for any obstructions.
To perform the test, a small tube (catheter) is inserted into the woman's uterus. Then, contrast is sent through the catheter into the uterine cavity and the fallopian tubes. In the meantime, X-rays are taken.
Lastly, it's important to confirm that the woman is ovulating. This can be achieved with a detailed medical history, testing urine for the telltale luteinizing hormone surge or by testing blood levels of progesterone after presumed ovulation.
Whatever the diagnosis is, treatment helps couples conceive more quickly and easily.
Treatments for infertility
Artificial insemination
For unexplained infertility, artificial insemination is an effective treatment. On the day of ovulation, the male partner collects a fresh semen sample. The sample is then washed. In this process, the volume is concentrated and the dead and abnormally shaped sperm are removed. Then, the sperm is put in a catheter and the sample is placed directly inside the female partner's uterus. This is painless and only takes a few minutes to do in the doctor's office.
IVF
For severe male factor or tubal factor infertility (when the fallopian tubes are blocked), in vitro fertilization (IVF) is often recommended. A woman is given hormone injections to help her mature multiple eggs simultaneously. The eggs are then removed from her body with a minor procedure done under anesthesia with ultrasound guidance. In the laboratory, the eggs are identified and counted and then fertilized with sperm.
If it is a severe male factor, the embryologist will inject one sperm into each egg to ensure fertilization. The embryologist checks to see which eggs have fertilized normally the next day. The embryos are then grown, to see which of them develop to the blastocyst stage. By reaching this milestone, the embryo is more likely to be viable.
Many embryos will stop growing before reaching this stage. Testing of embryos to determine if they are genetically normal or carry a disease is also an option. This enables doctors to select a genetically normal embryo to use for pregnancy.
Women who are 35 and older are at much higher risk for abnormal embryos (such as Down syndrome), so embryo screening is often recommended. After preparing the uterus for pregnancy, a woman undergoes transfer of her embryo. The embryo is placed in a catheter and this is used to transfer the embryo into her uterus. The procedure takes minutes, and success rates with IVF are very high.
As I have seen in my practice at Yale Medicine's Greenwich Fertility Center, with multiple treatment options, many couples are able to conceive and have a healthy baby.



